Basal Ganglia Lesions After CO – More than Movement
Basal Ganglia Lesions after carbon monoxide poisoning cause more disability than disfunction related to movement.
We have mentioned in several blogs that one of the long term effects of carbon monoxide poisoning can be basal ganglia lesions in the brain. We have also addressed many of the long term symptoms which can arise due to carbon monoxide poisoning. One of the most recognized conditions of carbon monoxide poisoning is damage to the basal ganglia lesions which form as a result of both hypoxia and the inflammatory effects of the reaction to the poison.
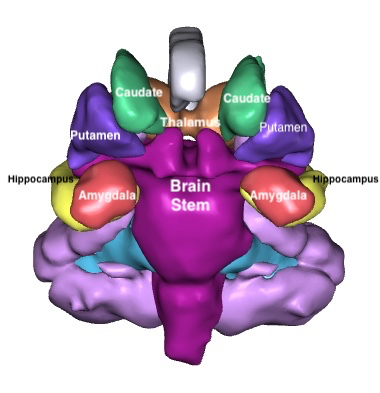
Shown here are the basal ganglia and there relationship to the brain stem and the hippocampus and amygdala. This is a coronal view, as if looking straight at the face.
The basal ganglia are associated with motor control which also expands to include motor learning , executive functions, behaviors and emotions. The basal ganglia are involved in the fine tuning of many voluntary motor functions, a control center adjusting and modulating signals to the skeletal muscles via the cranial nerve nuclei and spinal nerves.
Other functions deal with our processing of rewards and modulation of addictive behavior as well as language processing, learning, goal pursuit, decision making, eye movement, motivation and emotional response. Because it is influenced by dopamine it helps determine the level of euphoria we may experience from rewards such as sex, drugs and other external stimuli and keep those in balance
The basal ganglia, according to the Physiopedia “ are a cluster of subcortical nuclei deep to cerebral hemispheres. The largest component of the basal ganglia is the corpus striatum which contains the caudate and lenticular nuclei (the putamen, globus pallidus externus, and internus), the subthalamic nucleus (STN), and the substantia nigra (SN).”
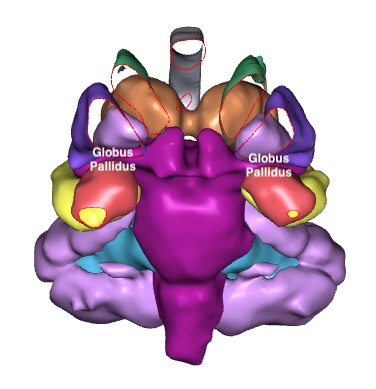
Basal ganglia lesions can occur after carbon monoxide poisoning. Shown here is the globus pallidus as lesions there are quite specific for carbon monoxide poisoning. As can be seen, the globus pallidus is tightly tucked in among other structures, including the putamen which is cutaway here to show the globus pallidus.
When the basal ganglia are damaged after a brain injury such as carbon monoxide poisoning it can result in any combination of the following deficits.
Chorea can Occur as a Result of Basal Ganglia Lesions
Chorea is when small repetitive movements start in one part of the body and then randomly move to another part of the body. Chorea comes from the Greek word for “dance”. The person may appear to be restless, fidgety or dancing. These movements are completely unpredictable. Yet individuals with chorea will sometimes incorporate these movements with voluntary movements in order to appear normal.
Athetosis is a stream of writhing effects most commonly in the hands and feet, and in some cases in the arms, legs, neck and tongue. These are called athetoid movements and are slow and rolling movements.
Chorea and athetosis tend to occur together. Another type of chorea called hemiballismus involves the involuntary flailing of the arm in a violent manner.
There are a number of good videos on Youtube on brain anatomy in general and specifically about the basal ganglia. Linked here is one of the good ones.
Dystonia After Basal Ganglia Lesions
Dystonia consists of sustained, involuntary muscle spasms that can force people into unusual body positions. It most commonly affects the eyes, jaw, mouth, neck, arms and legs. Rarely it can affect the torso as well.
Segmental dystonia affects two or more adjacent muscle groups.
Parkinsons can Originate in the Basal Ganglia
Parkinsonism displays as a resting tremor, stiff muscles, slow or delayed movements, difficulty initiating movement, difficulty with balance, difficulty with walking and a shuffling gait.
People suffering from damage to the basal ganglia may also exhibit obsessive-compulsive disorder as the basal ganglia are also connected to the prefrontal cortex.
There are several treatments for helping manage these effects of damage to the basal ganglia. There are medications to manage muscle spasms such as trihexyphenidyl and baclofen. Botox injections are sometimes used to block signals to the affected muscles. In extreme cases surgery is an option. But the most common management is through neuroplasticity. Working with a neurologist and physical therapist to retrain the affected muscles and rebuild neural pathways.
Many of these effects of damage to the basal ganglia are painful as well as debilitating. Neuroplasticity treatment works on alleviating the secondary effects of basal ganglia damage, not the damage to the basal ganglia itself
Studies of basal ganglia damaged by carbon monoxide poisoning show a diminished perceptual organization and processing speed function. Carbon monoxide causes permanent brain damage and damage deep inside the brain may actually cause more global brain dysfunction than injury to the cerebral cortex.
As we have seen in the previous blog, many systems in the brain work at regulating the function of other elements, either enabling them or inhibiting them. The job of the basal ganglia is to fine tune the signals and responses. In the case of the basal ganglia it uses two pathways to process signals; the direct pathway and the indirect pathway. The direct pathway selectively activates certain motor or cognitive programs in the brain and the indirect pathway inhibits the execution of competing motor program.
The job of the basal ganglia is not to initiate motor programs but to regulate the execution of commands so that the particular command is completed without competing commands interfering with the actions for the task at hand. It basically acts like a gateway modulating the priorities passed down from the cortex.
It becomes more complex as there are certain cognitive functions that also look through the basal ganglia. Those are often cognitive functions having to do with motor learning and other functions which have a motor/cognitive interplay. This extends to tasks which require repeated trials and involve unconscious learning. Think of this as similar to muscle memory where through practice your muscles learn a task which then becomes automatic to us. And this works both ways that a cognitive stimulus might impact a certain correlation to a motor response. We might not be able to explain how we learn something through repetition but we learn it anyway.
Think of the basal ganglia as a sort of circuit board plugging in the correct cognitive and motor programs required to complete an action. Someone throws you a ball and aside from the action needed to physically catch the ball, you are using information about size, velocity, etc to perform that task so the basal ganglia is plugging in those programs to assist.
It is thought that obsessive-compulsive disorder due to damage to the basal ganglia may involve a lack of inhibiting certain actions which can be repetitive or in reverse, cognitive functions which become repetitive without an order to stop.
The basal ganglia is one of the least understood areas of the brain and it is through studies of movement disorders such as Parkinson’s Disease that insight is being gained. It is only recently that we are beginning to understand the link between the basal ganglia and emotions.
If we understand that motor responses to stimuli can involve an emotional component then this is easy to grasp. We react to pleasant and unpleasant stimuli differently. This response is divided into valence, which is movement toward or away from a stimulus, and arousal, which is the intensity of the emotional activation. The role of the basal ganglia in emotional response is very complex and reaches into the foundations of our understanding of morality and other abstract thought.
What is not fully understood about the basal ganglia is how it activates with the absence of motion as studies are only able to measure the cognitive and emotional components in the presence of a motor response. For example, test subjects pushing buttons in response to presented stimuli. It is generally presumed though that response inhibition is shared by all aspects including motor, cognitive and emotional response to some extent.
The basal ganglia are such a complex subject which is generally agreed to be understudied and much of our current understanding comes from animal models. It is really only through the study of movement disorders that we are gaining a clearer picture of the complexity of the basal ganglia’s role in all aspects of brain functioning. New advances in neurosurgery and electrophysiological are also advancing our understanding.
We are also beginning to understand that basal ganglia lesions are more likely in acute carbon monoxide poisonings where a more diffuse damage occurs through long time exposure. This is a significant finding in that arguments that damage has occurred over a long period of time may not hold up as an excuse for a severe case of carbon monoxide poisoning.
Of further note are studies that show that basal ganglia volumes may diminish over time after carbon monoxide poisoning.
According to a study by Hopkins RO, Fearing MA, Weaver LK, Foley JF, Brain Injury, March 2006; 20(3): 273–281.
Carbon monoxide poisoning results in basal ganglia volume reduction 6 months post CO poisoning. Slow mental processing speed and impaired memory correlated with smaller putamen and globus pallidus volumes. Clinicians need to be aware of basal ganglia neuropathologic changes in the absence of observable lesions following CO poisoning.
Their study found 28% of subjects had volume reduction in at least one basal ganglia structure by 6 month leading to a reduction in verbal memory and mental processing speed.
Similar findings regarding reduced volumes in the structures of the basal ganglia have been studied in cognitive disorders such as dementia with Lewy bodies (DLB) where memory was relatively spared while processing speed, attention and other executive functions were compromised.
This expands the scope of damage to the basal ganglia and its impact on not only the motor system but the executive functions as well. In addition, it opens up the connection between the delayed long term effects of carbon monoxide poisoning and decreased volumes in the structures of the basal ganglia in addition to the presence of lesions. Or more precisely, even in the absence of apparent lesions.
The basal ganglia may be one of the least understood structures of the brain but there is no mistake that acute carbon monoxide poisoning can cause permanent and far reaching damage to those structures. And that damage reaches out beyond motor impairments into almost all aspects of the brain’s function in ways we are only beginning to understand. Motor functions, cognitive functions, emotional responses, and behavioral responses relying on the ability of the basal ganglia to put all of the programs together to allow us to act, learn, commit to memory and more.
And so much more than its dictionary definition “a group of structures linked to the thalamus in the base of the brain and involved in coordination of movement.”
Not all CO Related Brain Damage Has Lesions in Globus Pallidus
Basal ganglia lesions have had outsized importance in the diagnosis of carbon monoxide brain damage because for a long time, it was believed that all of those with carbon monoxide poisoning would have basal ganglia lesions. That belief has resulted in a severe under diagnosis of permanent brain damage after CO poisoning. First, lesions deep inside of the brain can be subtle, with most neuroradiologists having little experience in calling CO poisoning damage. Too little time is devoted to reading clinical scans and these lesions are often missed. Further, imaging capacity has increased exponentially over the last decade but much of that technology is not used or understood in the clinical setting.
Better MRI Techniques Do More than See More Lesions
Increased resolution has identified more lesions. Increased lesions has helped differentiate abnormal signal in the basal ganglia that are often ignored. Further, smaller gaps between slices makes it less likely that a lesion, which may be smaller than the gaps between slices, may be missed. A 4 millimeter globus pallidus lesion could be significant, but most clinical coronal imaging has 5 millimeter gaps between slices. A 2 mm lesion would likely be missed. Often, coronal sequences, which are best to see these lesions, aren’t even done on many clinical scans.
Further brain volume can now be accurately measured using 3D MRI tools. A loss of volume in the basal ganglia may identify pathology even though a specific lesion or bleed might have been missed.
This blog was written by Rebecca Martin

Leave a Reply
Want to join the discussion?Feel free to contribute!