Long-term Problems Not Tied to the Dose of Carbon Monoxide
The dose of carbon monoxide in the blood, does not predict long term outcome once CO gets to a level where symptoms occur – 15% COHb. In the context of medicine/toxicology, the issue of how much of a toxin the body ingests, is often thought key to outcome. We often hear the term, severe carbon monoxide poisoning, used to classify those at the most risk for permanent damage from carbon monoxide exposure. However studies indicate that there is little difference in the possibility of permanent damage and ultimately deficits in the classic definitions of mild versus severe carbon monoxide poisoning. In fact, a COHb level of 15% is sufficient to result in permanent damage and deficits caused by triggering the immunological and inflammatory processes of the body. This can lead to permanent damage of the brain, heart or organs. The sequelae of carbon monoxide poisoning can typically arise two to 21 days after exposure, and up to five or six weeks after exposure. In some cases long term problems will not be recognized until a significant change is observed in functioning. Though we can, with certainty, predict the significant potential for long term problems due to carbon monoxide poisoning and that those deficits may be permanent regardless of the amount of exposure.
Carbon monoxide exposure can absolutely become lethal, but let us examine the symptomatology of carbon monoxide poisoning as experienced at the scene, during emergency treatment and post-exposure.
Dose of Carbon Monoxide - Symptoms Imperfect Correlation
One of the very first symptoms of carbon monoxide poisoning is a headache resembling a tension headache. Other initial symptoms are often difficult to differentiate from the flu. In the instance where more than one person is affected, food poisoning is often mistakenly suspected. Even though carbon monoxide poisoning can present with flu-like symptoms such as headache, muscle ache, stomach pain, nausea, vomiting, dizziness, shortness of breath, fatigue and confusion, there is a major difference between the flu and carbon monoxide poisoning: Carbon monoxide poisoning is not accompanied by a fever.
In the event these initial symptoms are mistaken to be due to flu or food poisoning and the affected person or persons remain in the contaminated environment, symptoms can quickly escalate and lead to more serious issues. The person might enter a mental state and show personality changes similar to intoxication. Dizziness will escalate to vertigo and the feeling the room is spinning. There can be ataxia, a disconnect between the brain and nervous system. Breathlessness and an accelerated heartbeat, tachycardia, may occur and even lead to angina or a heart attack. One might experience seizures as the brain experiences bursts of electrical activity. Ultimately unconsciousness and death may occur.
The onset of symptoms may be gradual or rapid. And because carbon monoxide poisoning can affect judgment, the escalation of symptoms may make it extremely difficult for the victim to assess the danger or seek help.
Other neurological symptoms might include loss of vision, or hearing, speech and language problems and memory/attention problems as well as a general slowdown of mental functioning and increasing confusion and disorientation.
How do we know we are experiencing the initial symptoms of carbon monoxide poisoning? First and foremost, if you suspect that carbon monoxide poisoning could possibly be the cause of symptoms, evacuating the area is the most important way to verify concerns. Don’t do the common sense thing of airing out a place you suspect of having carbon monoxide leak. Get out. The flu and food poisoning will not lessen when evacuating the area. In the time it takes you to air out the premises, you may pass out. You don’t know how much CO is in the air. It could be deadly levels. Do not reenter until emergency services have told you it is safe. Call 911. Do not try to self-diagnose. Leaving the environment is not the only treatment that may be needed and blood work will be needed to determine the levels of carbon monoxide and whether oxygen treatment is indicated.
There are other clues to whether or not the symptoms you are experiencing are from carbon monoxide exposure. If other people in the area are also experiencing similar symptoms that is the red flag that carbon monoxide is the culprit. Pets can be affected as well so pets may also be experiencing the same symptoms. In fact, pets are more susceptible and the smaller the pet, the more susceptible it is. A healthy pet’s sudden unexpected death can be a huge warning sign.
In our experience of the most deadly of CO cases, the pets are the canary in the coal mine. It is not just that they get sick quicker, because of smaller body weight and faster respiration rates. It is when CO levels (as opposed to dose of carbon monoxide[1]) get to the highest levels, they are often accompanied by unburned hydrocarbons, which a dog may in fact smell. If you are feeling ill and your dog is highly agitated, get out.
Winter is Worst Carbon Monoxide Season
Time of year is an issue as well as the majority of home carbon monoxide poisonings occur in the winter, especially when furnaces are first turned on. And there may be physical clues as well such as pilot lights which frequently blow out or yellow instead of blue flames coming from gas appliances. The message is, if you suspect that it might be an issue, take action to rule it out before it becomes lethal. And the first step is evacuation.
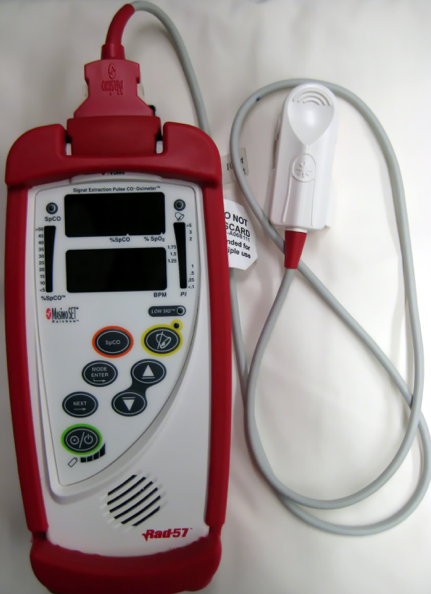
While Dose of carbon monoxide doesn’t predict long term symptoms, determining that poisoning occurred is important. One under used but useful tool to do so is this, Rad 57 finger tip carboxyhemoglobin saturation monitor with pulse c0-oximetry. This pulse CO-oximeter is manufactured by Masimo. Photo ©James Heilman, MD. https://commons.wikimedia.org/w/index.php?curid=8838592
It is extremely important to seek out medical care if exposure is suspected. A blood test is the most accurate way to determine the level of carbon monoxide in the blood, but finger probes, called pulse co-oximeters, are also diagnostic. These are similar to the pulse oximeters that are used to measure oxygen in the blood. The pulse co-oximeters also measures CO.
Even in cases where it is suspected that a low level of carbon monoxide may be present, exposure over time can still cause permanent health issues and at the very least one should consult a doctor for further testing. Keep in mind that even what emergency personnel deem to be mild exposure can have permanent consequences. In this case, the home or workplace must still be inspected to determine whether it is safe to return or if there is an ongoing problem.
There is also the issue of the accuracy of blood testing. By the time you reach emergency care, the levels may have fallen and testing becomes inaccurate. This is why sometimes the pulse co-oximeters provide the most diagnostic COHb measurement. This is especially true of children. Children breathe faster than adults and their levels may drop quickly even though initial damage has occurred. And there may also be delays as children are not as cooperative with the blood testing procedure which creates further delays in discerning the level of carbon monoxide which may have been present.
In cases of CO exposure one might experience many of the symptoms of carbon monoxide poisoning which can combine to produce brain impairment, cardiac conditions, or organ damage or a combination of all of these and result in long term problems. These include neuropsychiatric issues which may result in a long term inability to concentrate or function at a pre-exposure level. In children, the full extent of these neuropsychiatric issues may not be determined because of the developmental level at time of exposure. These issues may not surface until future developmental milestones in brain development are reached, such as puberty. As the dose of carbon monoxide is far less predictive of brain damage than most medical personnel think, the underdiagnosis of permanent problems in those whose testing shows COHb levels around 10% or below, is legion.
A family may not see the patterns of neuropsychiatric malfunctions until a child returns to school where their performance may show negative changes. A teacher may complain of the child’s inability to concentrate or a drop in grades. An adult may not be aware until returning to work and finding that focus, concentration or memory become not only impaired but also find that routine tasks are resulting in frustration and fatigue which can become debilitating. All of these ongoing symptoms can lead to other psychiatric issues as well as school or job performances spiral lower. Depression and anxiety may result.
Scientists have recently determined that not only is the ability of the blood to carry oxygen impaired during carbon monoxide poisonings but also the cells of the organs the blood is being delivered too. This can result in changes in the heart, brain or organs which makes their cells less receptive to receiving and utilizing oxygen in an efficient way. This can create a cycle of functioning that is virtually defeating the body’s ability to heal and return to normal functioning. This inability to absorb oxygen becomes a permanent dysfunction which can in turn cause other issues.
One of these issues is inflammation which occurs as a result of continuing damage caused by cells which are no longer functioning at a pre-exposure level. The body attempts to correct the damage by throwing more oxygen at the damaged areas. However the human body requires a mix of gases to function and break down the oxygen it is receiving. It does this by using carbon dioxide to help break down the oxygen for use. The body malfunctions and creates inflammation which ultimately causes more damage. The body then attempts to correct his and the result is a loop of damage which may arise weeks after the exposure.
We know that carbon monoxide attaches to the hemoglobin more readily than oxygen. But we are now learning that the components of hemoglobin itself react in different ways and ongoing studies are determining what impact each of the components of hemoglobin may be impacting the cells they come in contact with.
One of the possible outcomes of carbon monoxide is the development of Parkinsonism. This is a clinical syndrome which is characterized by tremors, rigidity, postural instability and slowness of movement or bradykinesia. A 2015 study, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4602584/ showed a significant connection between carbon monoxide poisoning and Parkinsonism. Additional studies have found correlations between the onset of dementia and former carbon monoxide poisonings.
As we continue to delve into the functions of the human body we are finding long term health issues that may persist beyond weeks and into years after the exposure. particularly as relates to the functioning of the brain and nervous system. And just as our exploration into the long term effects of brain injury, we see more and more connections between compromised brain function and carbon monoxide poisoning.
Disability in those Who Survive
Carbon monoxide may be invisible but it impacts the human body in ways that we are constantly discovering as new scientific research is done.
We are entering another winter season when carbon monoxide injuries and fatalities tend to rise. We also looking at another possible Covid 19 lockdown and spending more time at home or in enclosed spaces. This is a time for absolute awareness that carbon monoxide is deadly and at best can result in other health issues. And it is preventable on every level. Whether it be that vacation hotel trip, or a hunting weekend at a cabin, or just time spent at home with family–awareness to the danger of carbon monoxide poisoning and a familiarity with potential symptoms could save countless lives. Know the symptoms and be cautious when discounting symptoms as just the flu, or just a bout of food poisoning. Better safe than sorry were words written to particularly suit carbon monoxide awareness. If in doubt, evacuate immediately, seek care, and do not return until the area has been inspected for safety.
Make sure you have a functioning carbon monoxide alarm, everywhere that you are indoors. Having an outdated alarm on the ceiling or one that doesn’t have batteries that work, won’t help. Our advice: get a new combination smoke/CO alarm, one with a sealed, ten year batteries.
Becca Martin authored this blog
[1] When we are talking about dose of carbon monoxide we are talking about the concentration in the blood, not in the ambient air. How high the dose of carbon monoxide becomes will be dependent on how high the ambient air level is, how much of the CO a person (or pet) breaths. The faster the mammal breaths, the faster the dose of carbon monoxide will climb.

Leave a Reply
Want to join the discussion?Feel free to contribute!