Carbon Monoxide Physiology – In Words and Pictures
To being our topic of carbon monoxide physiology, we must go back to Claude Bernard, a 17th century physiologist who first discovered the affinity of carbon monoxide for hemoglobin and the mechanics of the toxicology which results. With coal coming into the picture as a primary source of fuel and the invention of the internal combustion engine the science of health turned its attention to the effects on the population. Seventy-five years after Bernard’s initial findings, Warberg used yeast cultures to prove that not only did carbon monoxide inhibit the transport of oxygen via the hemoglobin but it also inhibited the intake of oxygen by cells.
As carbon monoxide physiology was explored, it was quickly determined that not only did carbon monoxide have a far greater affinity to hemoglobin, it also was able to bond in a more perfect way than oxygen. This made carbon monoxide a deadly asphyxiant as it was able to quickly block the absorption of oxygen at high concentrations. By blocking the oxygen absorption of the cells, it was also able to cause tissue damage and a resulting inflammation which could have long range effects. The great affinity of carbon monoxide for hemoglobin (210 times greater than oxygen) is only surpassed by its affinity to myoglobin. When carbon monoxide binds to cardiac myoglobin it can cause depression, hypotension and arrhythmias. This can result in further hypoxia and ultimately death.
The carbon monoxide bonds with the mitochondrial cytochrome which can lead to demyelination in the brain. One of the most understood areas of pathology associated with carbon monoxide poisoning is its effect on the basal ganglia because of their high oxygen consumption. Other common areas of impact are the white matter, hippocampus and cerebellum.
If a survivor has lesions or structural abnormalities in the basal ganglias, particularly the globus pallidus, then it is probable that the cause was carbon monoxide. Only a few other pathologies are on the differential diagnosis, and if there is CO poisoning and no other severe ischemic mechanism, then even the neuroradiologist may be able to conclusively link the MRI abnormality to the poisoning.
But keep in mind the difference between a finding being specific for carbon monoxide poisoning and the absence of that finding ruling out poisoning. See Hopkins, et. al. While almost everyone with basal ganglia abnormalities post CO exposure will be diagnosed with CO brain related brain damage, not everyone who has CO related brain damage has globus pallidus lesions. Even in severe poisoning cases, more than half of the survivors did not have basal ganglia lesions.
The basal ganglia are typically associated with movement but encompass other functions such as motor learning and movement choices which facilitate desired movements and movements which avoid adverse stimuli. It’s a complicated network which controls our ability to perform actions, or block actions. To simplify; you reach out to pick something up, you realize it’s a spider, you withdraw your hand…that is your basal ganglia at work.
Carbon Monoxide Physiology – Basal Ganglia, Hippocampus and Amygdala
The noteworthy subcortical structures (beneath or inside the cerebral cortex) are the basal ganglia, the hippocampus and the amygdala.
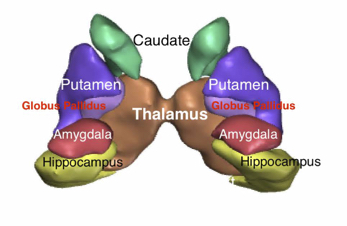
The basal ganglia consist of the caudate, putamen, and globus pallidus. The basal ganglia cross into both the midbrain and to the subthalamic areas. The basal ganglia are closely interconnected with the cerebral cortex, thalamus, and brainstem, as well as several other core brain pathways. The basal ganglia contribute to control of voluntary movements, procedural learning, habit learning, eye movements, cognition, and emotion. It is the connection of the sensory pathways to the basal ganglia that makes them so central to so many functions. The basal ganglia are one of the central interchanges of the brain, as core to proper information traffic flow as the interchange between two major interstate highways.
The Putamen and Globus Pallidus Pathology
The putamen and the globus pallidus combine to make a structure that looks something like a lima bean. When the early anatomists dissected this part of the brain and looked at these two structures together, they decided it resembled a bean. These two structures stand out together on autopsy because they have more gray matter. Thus collectively, these two structures have been referred to as the lentil, for bean.
The figure below shows the Lentil, consisting of the outer Putamen and the inner Globus Pallidus.
An understanding of the physiology of carbon monoxide poisoning should include an understanding of the limbic system.
The outer side of this lentil is the putamen and the inner side is the globus pallidus. Thus, in two-dimensional anatomy diagrams of the subcortical structures, the globus pallidus appears hidden, because it is on the inner side of the bean.
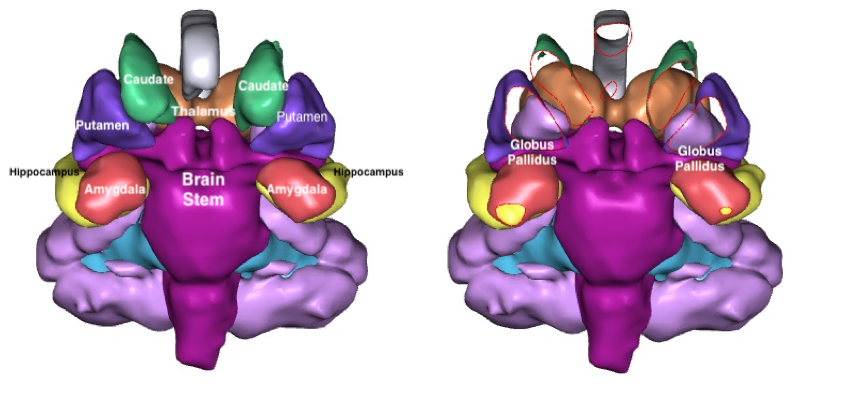
Two different views of the coronal view of the subcortical structures are shown. In the picture on the left, the Putamen obstructs the Globus Pallidus. The image on the right has been sectioned so that the inner structure can be seen. The Globus Pallidus is a light purple, where the Putamen is dark purple, the Caudate is green and the Thalamus tan. The Globus Pallidus is a triangular structure seen on both the coronal and axial planes, sandwiched between the Brain Stem, the Thalamus, the Putamen and the Caudate.
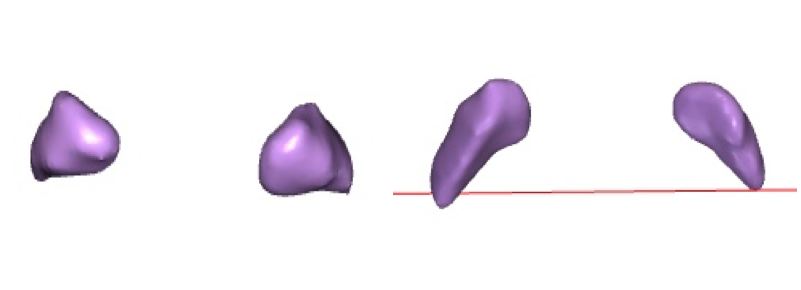
The globus pallidus is shown by itself in a coronal view on the left and an axial view on the right. (The red line is the sectioning mark in the program.) The globus pallidus is triangular in both views.[2]
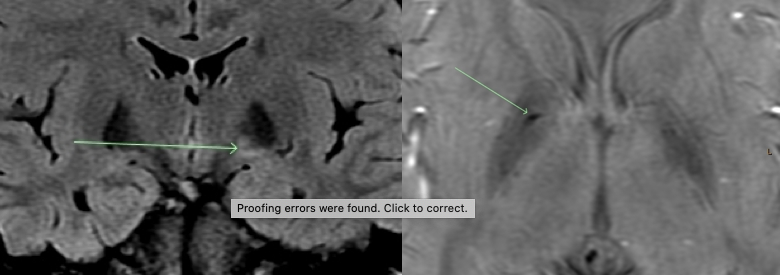
Different views of the same lesion in the globus pallidus are shown on an MRI
While not everyone who has carbon monoxide related brain damage will have visible lesions on MRI in the globus pallidus, it is clear when lesions show up in here after a poisoning, that they were caused by carbon monoxide. The reasons that the differential diagnosis for globus pallidus lesions is almost always CO poisoning is multiple.
First, the exposure to CO poisoning has probably already been established from extrinsic facts, such as ambient CO levels or abnormal COHb levels. Second, the globus pallidus is fairly immune to most mechanical forces of trauma. It is buried deep within the brain protected from most contact phenomenon. Any rotational force that would impact the globus pallidus is likely to also impact the brain stem, resulting in significant coma or death. Further, the globus pallidus is an area of the brain that has constant information flow through it, meaning its need for blood flow is intense. Finally, the globus pallidus is highly vulnerable to any pathology as the entire structure is too small to work around any pathology. Evolution buried the basil ganglia out of the way of clubs and falls for a reason.
White matter provides a communication relay between different areas of the brain. The hippocampus has a major role in learning and memory. The cerebellum has a big part in the planning and execution of movement. While this is a very simplified look at the functions of the parts of the brain that can be most affected by carbon monoxide, the overall picture is of diverse parts of the brain working in conjunction with each other.
Click here for a further treatment of brain damage from carbon monoxide poisoning.
There can be a difference in the effects of exposure to low concentrations over a period of time and exposure to high concentrations in a short period of time. In low-level-long -term exposure, the effects may seem to resolve as soon as the person is outside of the environment. exposure, the effects may seem to resolve as soon as the person is outside of the environment. Those with repetitive exposures, particularly where the repetitive exposures would have exceeded 10% COHb concentrations can have serious brain damage – that the repetitive brain trauma may have worse consequences than a single higher dose. This is likely due to similar phenomenon as makes multiple concussions in the same time period so disabling.
Generally, there is about a 40% risk of long-term brain damage. Thus, if you expose five people, two may have permanent brain damage. But if the same five people are exposed to a bad furnace for weeks, then it may be that everyone has brain damage.[2] These problems can include a greater vulnerability to higher levels of carbon monoxide.
Exposure to high concentrations of carbon monoxide can very become life threatening toxicity. In cases where portable electric generators are the source of the CO, victims often “drop where they stop.” Once consciousness is lost in such an event, death may quickly follow. This is due to its exceptionally high affinity for the hemoglobin, which not only blocks oxygen, it makes a more efficient attachment. Our oxygen absorption is a process designed to sustain life but far from perfect as we are unable to glean oxygen for survival in the carbon monoxide model. Asphyxiation and death results if we are not reintroduced to an oxygen rich environment.
In cases of death, it is usually as a result of cardiac arrest. The heart doesn’t have enough oxygen to keep beating. The body soon dies.
Carbon Monoxide Physiology – Oxygen Administration
The use of oxygen to treat carbon monoxide poisoning was first explored by Claude Bernard. Early research was limited by the lack of access to a source of usable oxygen to conduct studies. It is a line of research that continues today as scientists explore different forms of oxygenation and delve into the effects of carbon monoxide on the different components of the hemoglobin itself. As we delve deeper into the actual structure of hemoglobin we discover new explanations for how it works and the impact each component has on different functions of cells and tissues. We are able to look at the inflammatory issues in greater depth and their part in long-term damage as a result of carbon monoxide poisoning.
A key to understanding carbon monoxide physiology is understanding DNS which is largely caused by inflammation and other immune responses. Inflammation is the result of our own body perceiving a threat and fighting back. Often this results in our own body fighting the healthy recovery of damage in a misguided attempt to eradicate the threat. We see an excellent example of this with the Covid virus, where infected patients’ own bodies go into overdrive to eradicate the virus and cause severe consequences. The mechanics of inflammation in carbon monoxide poisoning can also cause damage which may not be apparent until a period of time has passed. When this is occurring at the cellular level the impact on different functions may range from mild to severe depending on the cells and tissue affected. In carbon monoxide poisoning we see injury to the neurologic and cardiac systems. Delayed neurological sequelae can appear 3 to 240 following severe exposure. While myocardial injuries increase the risk of death from heart failure up to three times the rate of the healthy population.
There are more areas of the body which can be affected by severe exposure, however. It can impact the kidneys leading to renal failure. It can affect the electrolyte and glucose levels. It can affect the blood lactate level. Blood traveling to sensitive organs can bring injury as tissues are damaged by lack of oxygen and consequently faulty oxygen. We function on oxygen with certain levels of other gases like carbon dioxide which increase the rate of our oxygenation and those levels are normally in a balance meant to increase efficiency. When those levels are not functioning properly, decreased efficiency is a result which can further exacerbate the breakdown.
[1] These pictures are created in a program called Freesurfer from an actual MRI. The color coding is done in the program. The color coding here doesn’t have any special significance, other than distinguishing between this outer part and inner part of the lentil. These structures have complex networks the process and relay motor function, motor control and emotion.
[2] Understand of course that in any one family poisoning event, the statistical probabilities do not reach statistical significance, so that there may be no one with permanent brain damage or it could be one, two, three, four or five out of five with permanent brain damage. We have as many cases where people contact us after a poisoning and have a complete recovery as we do who need the remedy of a lawsuit to compensate for the long-term damage. The Brain Injury Law Group only undertakes litigation for those with permanent deficits and symptoms of CO poisoning.

Leave a Reply
Want to join the discussion?Feel free to contribute!