Carbon Monoxide in Children Requires Expert Assessment
This week I want to cover a difficult subject that has been interwoven into many of our blogs; the impact of carbon monoxide poisoning in children. Children and those with medically compromised health are at greater risk for carbon monoxide poisoning. Children are specifically at greater risk due to their higher metabolism. According to the National Institute of Health, approximately 1600 children are hospitalized annually for carbon monoxide poisoning. 5000 children per year seek medical treatment of some type for carbon monoxide poisoning. As we have noted previously, those numbers could be higher as there are cases where carbon monoxide poisoning occurred but was not suspected. Carbon monoxide poisoning is the leading cause of poisoning in children in the United States as well as globally. Carbon monoxide is also the leading cause of death in fatal poisonings.
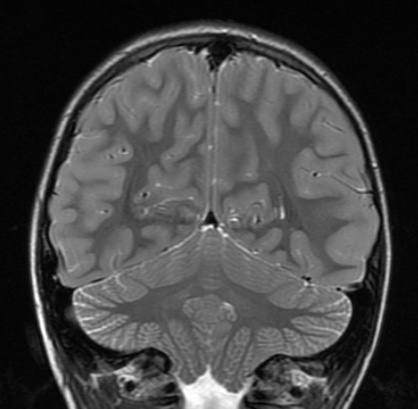
Assessing brain damage after carbon monoxide in children involves more complex assessment tools, from the ER all the way through adulthood.
There are many sources for carbon monoxide exposure which pose a risk to children. The most common cause is being exposed to a fuel-burning appliance like a furnace of boiler. And in many of those cases, improper maintenance, installation, use, or prevention can be found. Let’s focus on the dynamics of immediate inhalation of carbon monoxide gas, stage by stage.
In an earlier blog we had discussed the Boone Hotel incidents which claimed the lives of the elderly Jenkins couple and 11-year-old Jeffrey Williams. We had noted that in between the two incidents, the mothers of several girls attending a birthday party in the room above had gone to the hotel staff with concerns that the girls had fallen ill due to exposure to chemicals in the pool. The pool was examined and deemed safe and the girls’ symptoms were dismissed as possible food poisoning. Because carbon monoxide symptoms (nausea, headaches, dizziness, vomiting) can be mistaken for many things including food poisoning, viral infection, etc., it is extremely vital when these types of symptoms present themselves that medical care is sought out and a thorough interview ensues. Was there a possibility for exposure? Were others, including adults, impacted? And if there is a valid concern that carbon monoxide poisoning has occurred, then proper testing and treatment must be done. Adherence to these protocols might have alerted officials to a problem at the Boone Hotel and averted the tragedy of Jeffrey’s death.
COHb Assessment Different after Carbon Monoxide in Children
Children have faster metabolisms and more immature nervous systems. Carbon monoxide binds to the hemoglobin in the blood with an affinity more than 200 times that of oxygen. The binding of oxygen to hemoglobin creates condition, creates carboxyhemoglobin (COHb). When COHb rich blood is delivered to tissue and cells, it takes the place of oxygen, potentially asphyxiating the cells. As a result, tissue hypoxia occurs. This hypoxia is most evident in those organs with high metabolic demands, such as the heart and brain. When the immune system senses this poison, it begins to fight back. Inflammation can then occur resulting in temporary or permanent damage to the nervous system. And in children, the true extent may not be assessed until puberty and beyond.
Diagnosing carbon monoxide poisoning in children on the day of the event is more complicated than with adults because the children re-oxygenate the blood faster than adults do. The reason they do so is that they breathe faster. Respiration rate is directly related to how quickly COHb is removed from the blood.
COHb Half Lives are Shorter
However, because of a child’s higher metabolism, the carbon monoxide in the blood may be reduced quickly after removal from the source of poisoning so blood tests may not detect the extent of the poisoning or potential damage when presenting at the emergency room. And also, due to the nature of children, getting a timely blood test done may factor into the diagnostic process. Children are not the most cooperative patients when needles are involved.
Think of respiration as opening a window to allow poison and then later fresh air in. During the poisoning event, the faster the respiration (the wider open the window) the faster the CO builds up in the blood. After the poisoning, the faster the respiration, the faster the CO gets out of the blood. Thus, if you test a family all expose to the same level of ambient CO in the air, at the moment of the peak CO concentration, the smaller the child, the higher that person’s level will be. In contrast, COHb blood measurements are always done hours after the survivors leave the poisonous air, sometimes several hours later. An adult’s COHb level will halve about every four to five hours (called a half-life.) Children may have half-lives,much shorter than that. The half-life of a child on oxygen may be under a half an hour.
We have seen a family where the adult levels taken two hours after the event were 15, the teenage girl 9, and her four-year-old sister 3. This is exactly what we would expect to see.
The most common symptoms which should arouse suspicion, but are not immediately conclusive, are nausea, vomiting, headache, fatigue, dyspnea (labored breathing), confusion, abdominal pain, visual changes, chest pain and ultimately, unconsciousness. Nausea and vomiting are the most frequently reported. Other symptoms can include, weakness or clumsiness, fast or irregular heartbeat, or loss of hearing. Severe cases present with a Glasgow Coma Scale (GCS) of below 8, altered mental state, unresponsiveness, cardiac arrest, respiratory failure and/or seizure. A GCS below 8 indicates severe injury and is based on scores for eye opening, verbal response and motor response.
The biggest clue to these non-specific symptoms being the result of poisoning is the timing of multiple people getting sick. Only an environmental exposure would explain multiple people getting sick simultaneously. While food poisoning is the other possibility, CO should be considered and if there is a fuel burning appliance as an explanation, 911 must be called. We have been involved in several mass poisoning events, where more than 100 people were poisoned at once. In each of those cases, it was when the second person passed out that the CO cause was suspected.
If your child exhibits any of these severe symptoms, and carbon monoxide is a potential risk, immediately remove your child to an area with fresh air and call 911. Always exit the premises before you call 911http://carbonmonoxide.com. If the poisoning levels are extreme, you might pass out before you finish the 911 call. We have had that happen too. Also never open the windows and doors and wait inside for EMT’s. Leave the premises unventilated and get out. A ventilated premises may misdirect the EMT’s from the CO diagnosis.
Brain Damage Behavioral Issues
Children are not just smaller adults and carbon monoxide can leave them with more complicated brain damage than adults. Further brain damage in children is not just a different category than brain damage than adults, but multiple different categories. Damage to the developing brain comes with infinitely more presentations than it does in mature people, as it directly impacts and can interfere with the maturation process. A fetus is horribly vulnerable. An infant may fall far behind benchmarks. A toddler may be impacted as they learn to walk or talk. A grade schooler will have additional challenges as the parts of their brain that are damaged may interfere with verbal learning. Fine motor coordination can impact not only school but play.
The most dynamic change may be in those transitional years between pre-teen and young adult. The frontal lobes are the part of the brain that evolve in those years, evolved because of the lessons and social interactions that become so challenging for all middle schoolers. Children learn to become adults in their frontal lobes and if the processes are disrupted, maturation set back. Mood and hormones are so challenging for all at this age. Add the burden of cognitive struggles and mood disorders can destroy relationships. I have often talked about the struggle for identity that comes after brain damage. When the identity is just being formed, that struggle is intensified.
Future Needs for Care
Often the biggest component to damages in a personal injury case are the economic damages that come with future care needs. Too many children with brain damage never develop the executive functioning skills where they can live independently. Getting along with their parents becomes so much more difficult but getting along without them may be impossible. What are executive functioning skills? I have written much about this over the decades of my web advocacy for brain damage, but essentially they are the skills that adults do differently than children. Adults need to self-regulate their behavior. Adults need to make plans. Adults need to initiate when to start a behavior, how to exercise it and how to complete it. So often, executive functioning involves a break down in that process.
Frontal lobe functioning also involves learning, memory and integration of new information into the collective individual maturation experience. Specific lesions to brain regions, can disrupt that. Interference with axonal development and communication can completely distort the process. The axons are the connections between different groups of neurons within the brain.
Most have heard stories of overt misbehavior after brain injury which can happen in those first few months after brain injury. Yet, even when the violent tendencies fade, the anger, irritability and rapidly cycling moods make relationships difficult. But the omission aspects of behavioral changes are clearly a challenge for relationships as well. Without initiation, motivation, planning and follow through, the survivors life will lack any vitality and the caregiver may just give up having to interact with an adult as if they were an eight-year-old child.
The core of behavior begins in our frontal lobes, as this is where we learned to become adults. As we reach puberty, the frontal lobes are still growing. The frontal lobes still have “empty hard drive space” to absorb the complicated nuances of human interaction. They continue to change and evolve long after most of other cognitive abilities are largely set. We learn math and reading skills in early grade school yet getting along at work can be substantively different at 30 than at 20. There is certainly no question that the behavior of a 30-year-old lawyer is dynamically different than that of someone in their first year out of law school.
Frontal lobe injury can clearly manifest itself in the following symptoms:
- Executive functioning disorders;
- Delays or failures of complex processing;
- Mood and emotional changes, otherwise called neurobehavioral changes;
- Impulsivity
- Decision making
- Loss of Maturity and
- Loss of insight;
This is not an exhaustive list. The frontal lobes make up largest portion of the brain and contain much of what makes humans different from other mammals. The frontal lobes are the “hard drives” for learning and behavioral memory storage. Focal injury to the frontal lobes can impact a wide variety of thought, memory and behavior. Further, damage to the white matter of the frontal lobes – the neuronal connective tissue underlying the outer layers of the cerebral cortex can have even comprehensive impact.
Never presume that a child has had a full recovery from brain damage because they are not exhibiting specific cognitive or emotional symptoms at a given age. Certain areas of the brain are not challenged before middle school years. So, what seems like a full recovery at 10, may seem very different at 13. Likewise, inability to transition into independence may not become apparent until 18-22. A child may grow to number one in his or high school class but have major compromises when expected to live independently of parents. Brain damage in children is a longitudinal process to assess.
But there is also a flip side to that. As the brain is still developing, brain plasticity, the process of getting a different part of the brain to take over tasks done by a damaged area has more chance in children than adults. The concern, however, is that plasticity can also work in negative ways and then brains internal organization may be thrown off.
So many carbon monoxide events involve children because homes and schools are often the place where the poisoning occurs. Children require a more careful acute examination and greater assessment of the brain damage that might have occurred.
Becca Martin contributed to this blog.

Leave a Reply
Want to join the discussion?Feel free to contribute!